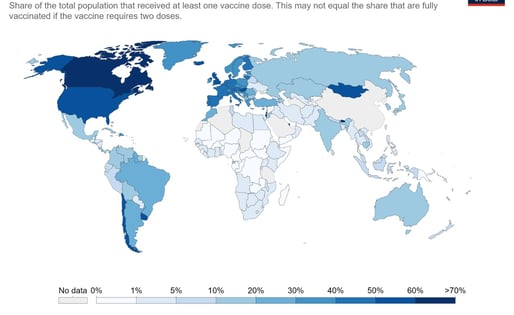
Broken DNA of Global Health Security
The COVID-19 pandemic has revealed that the extant global health security infrastructure is grossly inadequate. The current crisis has uncovered critical deficiencies in preparedness and response to epidemics and the predictive inability of current indices, underscoring the need for new framework and metrics. This paper argues for the global community to treat pandemics as a threat to global security to ensure mustering of political will and financial resources and to organize appropriate, rapid, and sustained domestic and international response. A public-health-only approach without commensurate national and global security measures will continue to fail to prevent local outbreaks from becoming global catastrophes. A values-based geopolitical order with resolute global leadership, political will, sustainable financing, and solidarity is critical for the world’s future.
This brief examines the nature of the threat from pandemics, the blind-spots in global health security that were revealed by the pandemic, and why a values-based geopolitical order is critical for the world’s future. It makes a case for the global community to treat health crises, such as the COVID-19 pandemic, as global security threats—this will help ensure the mustering of political will to organize appropriate, rapid, and sustained domestic and international response.
The Case for Securitising Pandemics
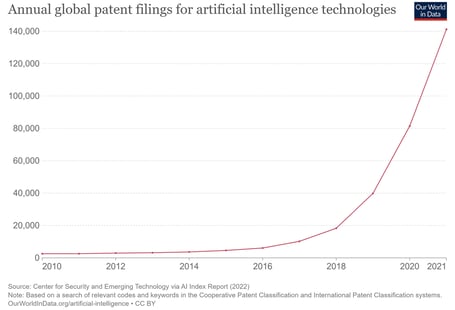
Artificial intelligence (AI) is being rapidly integrated into healthcare with a naïve belief in the objectivity of AI and a complacent trust in the omniscience of computational knowledge. While AI has the potential to transform healthcare, there are significant ethical and safety concerns. The pace of AI development and the race for AI supremacy is leading to a rapid, and largely unregulated, proliferation of AI applications. This paper explores the issues related to reliability, transparency, bias, and ethics to illustrate the ground realities and makes a case for developing standards and regulatory frameworks for the safe, effective, and ethical use of AI in healthcare.
Artificial Intelligence and the Myth of Objectivity
In the recent years, the abilities of artificial intelligence (AI) to augment those of clinicians have been repeatedly and emphatically demonstrated in many medical domains. However, the current state and nature of the technology have raised several concerns about its safety and ethicality. World Health Organization (WHO) has cautioned about the need to demonstrate evidence-based benefits before AI services are offered to patients as they may come with long-term risks. While AI brings immense possibilities, it is essential to address these ethical challenges to ensure its safe, reliable, fair, and trustworthy application in healthcare. This paper explores the challenges for AI in healthcare and discusses its ethical implications using the framework of the four core principles of modern bioethics.
Beyond algorithms: Ethical implications of AI in healthcare
Global Viral Hepatitis Strategy: Issues with Hepatitis B Immunization in India
Hepatitis B vaccination, a key component of the recently adopted Global Viral Hepatitis Strategy, has been plagued by various issues since its introduction under the National immunization program in India. While the concerns relating to the inclusion of the vaccine under the Universal Immunization Program, the vaccination strategies adopted and prevention of mother to child transmission of hepatitis B have been largely resolved, data from recent research has underscored the need for regular monitoring of immunological and epidemiological outcomes of the vaccine. Controversies surrounding the safety and efficacy of the recently introduced combination pentavalent vaccine have highlighted that besides reinforcing surveillance of adverse events following immunization in the public sector, the private health sector in the country needs to be supported in this activity by increasing awareness and strengthening public-private collaboration.
Need for tele follow-up – a study at a public sector quaternary referral hospital in India
The All India Institute of Medical Sciences (AIIMS) is the apex super-specialty, quaternary referral hospital of India. Its outpatient departments (OPDs) handle over 2.5 million patients every year, a large proportion of whom travel up to 2500 km for treatment because specialist facilities are not available in their regions. We conducted a descriptive study of 58 AIIMS faculty staff members, using a self-administered questionnaire followed by interviews with selected faculty members. During the year 2006, a total of 2,566,492 patients attended the various OPDs at the AIIMS, of whom 1,427,466 (56%) were old patients, i.e. they attended the OPD for follow-up. The questionnaire responses revealed that 55 (95%) of the respondents routinely provided follow-up medical advice to their patients using the telephone, email and/or letters. Only 3 (5%) respondents stated that they did not use any such means for follow-up of their patients. Most of the respondents identified benefits in the use of telemedicine and did not envisage any major difficulties in using it for the follow-up of patients. If appropriate tele follow-up facilities were available, probably more than one million OPD visits could be avoided annually at the AIIMS.


